On the frontlines
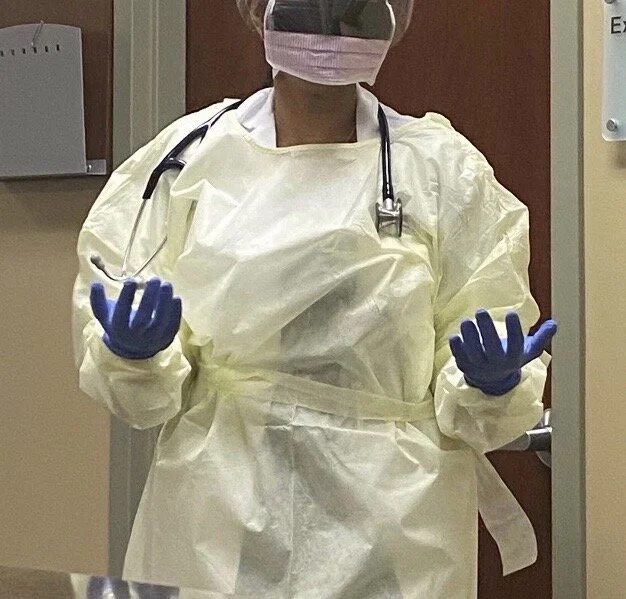
A Northview parent shares her experience working in the healthcare field during the coronavirus pandemic.Northview parent Annie stands in full protective equipment as she heads to treat another patient.
Photo: Special(Provided by anonymous source)
Grace Peng, News Editor & Rachel Everett, Staff Writer
*Annie is an alias chosen by the Messenger staff to protect the identity of an individual who has chosen to remain anonymous.
While others have yet to wake for another five hours, one Northview mom is already up, ready for another day of work at the frontlines of a rapidly growing pandemic. She is Annie*, a family practice physician in one of Atlanta’s biggest hospitals. Annie’s experience fighting the virus is evident in herself, as well as her family.
“It is overwhelming, but at the same time, we have the urge to help people. I want to help people, but unfortunately most of the time we don’t find a method to bring people back to life. It is unbearable to see so many people losing their lives,” Annie said. “I feel helpless.”
To say that the COVID-19 pandemic has taken the world by storm is an understatement. Georgia is no exception, with nearly 2,000 cases in Fulton County alone. The viral images of reused, spit-filled masks, cheek scars from goggles, and trash bins full of rubber gloves across social media and news networks are commonplace at Annie’s hospital. Like many hospitals across the nation, it is becoming increasingly overwhelmed, getting numerous calls from patients across the state regarding symptoms and the possibility of testing positive.
But the task of answering said calls is not limited to administration. Each call is a new source of concern for doctors and a race against time to find a solution to each individual problem, so much so that the hospital has established a new system of telemedicine.
In the new screening process for COVID-19, phone calls have become the new norm, replacing traditional walk-in visits or appointments. Patients are asked about their symptoms by phone and sent to coronavirus testing centers if they check off enough boxes. Although depending on electronic information and long-distance patient care is inconvenient, it is the only way to prevent hospitals like Annie’s from being overrun.
Although online appointments with doctors are much more common, the offices themselves are busy as well. For healthcare workers, breaks are now a rarity. The lack of personal protective equipment, or PPE, and medical personnel in many hospitals makes each interaction with patients more dangerous, as workers can easily become infected.
“We don’t have enough protective gear to see patients, sending them to outpatient centers, and trying to see healthy patients in the office. With a lot of health care workers being laid off, it is becoming very difficult to work efficiently,” Annie said.
While she is required to wear protective equipment when in the office, Annie, like many others, has been struggling to obtain masks for herself and her family, especially since the CDC has confirmed that the virus can be spread by air. Because Annie’s hospital has run out of N95 masks, doctors and other healthcare workers have resorted to wearing surgical masks, which offer a lesser degree of protection. She has only been able to secure four masks-one for each member of her family to use and reuse.
“If we go outside, my mom makes me wear masks and gloves, and I don’t like masks, especially because they’re surgical, not the N95 ones, and I’m literally breathing in my spit,” Annie’s daughter, a Northview sophomore, said. She also has another daughter who is a junior.
Annie herself is lucky enough to have tested negative, despite being in the presence of so many COVID-19 patients. The results of her test came back within three days, but many are less fortunate. Although test results can come back as soon as 48 hours after a test is taken, they can also take as long as 11 days. For medical personnel who test positive, the protocol is for them to retreat to quarantine for 14 days and have their workspaces closed and disinfected. Annie and her family members have experienced, firsthand, the toll the healthcare industry has taken as a result of the pandemic.
“Nothing has changed for me really, but I have to see her wearing all of this protective equipment when she goes to work. The only good thing is that she gets to come back earlier in the day,” Annie’s daughter said.
However, there is no knowing when there will be a spike in the number of coronavirus cases that will call Annie back to the hospital. The increasing rate at which infected patients are visiting means she will have to be at the hospital for longer hours than she already has.
“I will have to work more hours and try to bring in more doctors. The hospital will hopefully provide enough personnel to handle the patients or direct them to other providers,” Annie said.